CDC warns emerging fungus can cause severe, deadly infections in hospitals, nursing homes

CDC warns emerging fungus can cause severe, deadly infections
U.S. health officials are warning hospitals about an emerging and potentially deadly fungus, known as Candida auris, or C. auris, that is spreading in health care settings like ICU's and nursing homes, infection patients who are already battling severe health problems.
ATLANTA - The Centers for Disease Control & Prevention says Candida auris, or C. auris, is an emerging health threat, a type of fungus can cause severe, potentially life-threatening infections in people hospitalized with compromised immune systems.
Dr. Jose Vasquez, chief of infectious diseases at the Medical College of Georgia at Augusta University, says there are several reasons for concern about this fungus.
"The biggest fear is that it is multi-drug resistant," he says. "So, it is resistant to many different drugs."
The CDC says most C. auris infections respond to antifungal medication, but some do not.
Vasquez says C. auris is also hard to detect without highly specialized lab equipment that many hospitals do not have.
And, he says, it is hard to stop the fungus once it gets into a hospital setting, such as an ICU or nursing care facility.
C. auris can live on a person's skin without causing symptoms, allowing it to be transmitted from one person to another, or to get into a patient's body through contaminated surfaces or medical equipment like mechanical ventilators, feeding tubes and central lines.
'It is one of the Candidas that lives the longest on a surface, and we're talking about weeks," he sys. "So it can live there, dry and desiccated. Once it gets there, it kind of sets up shop, and it is very, very difficult to eradicate."
In 2022, the CDC says, Georgia had just 12 lab-confirmed C. auris cases, but Florida had 349.
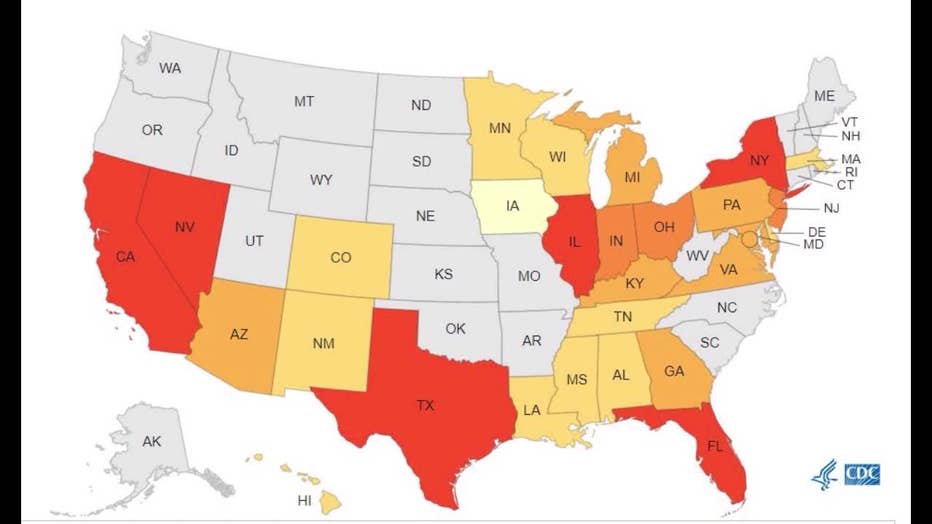
(Centers for Disease Control and Prevention)
Last year, the US reported 2,377 clinical C. auris cases, based on lab-confirmed cultures, and 5,744 screening cases.
Screening cases are swabs collected from patients to determine whether they are carrying the fungus anywhere on their body, although they are not experiencing signs of an active infection.
Dr. Vasquez believe there are many more cases going unconfirmed, and the pandemic may have fueled the spread of the fungus in healthcare settings.
"A lot of patients that had COVID ended up in the intensive care unit," Dr. Vasquez says. "Many patients ended up on mechanical ventilators. Those are all risk factors for Candida: (being in) the intensive care unit, on ventilators, on antibiotics or one centralized lines for a prolonged period of time."
C. auris can cause bloodstream, wound and ear infections, triggering fever, chills, and, in some cases, septic shock, he says.
DANGEROUS PLANT FUNGUS INFECTS MAN IN FIRST-KNOWN GLOBAL CASE, DOCTORS SAY
The CDC says, based on the limited information available about C. auris infections, about 30% to 60% of patients infected die, although most are already dealing with severe illnesses that can undermine their body's ability to fight infection.
Still, Dr. Vasquez says, C. auris not contagious or a health threat outside of healthcare settings.
"So it's not like you, or I are going to be walking down the street, and say hello to somebody, and shake hands (and get infected)," he says. "That's not going to happen. You have to be in the hospital, and then you have to have the risk factors which I mentioned: they are on broad spectrum antibiotics, or they're on mechanical ventilation, or they've been in the intensive care unit for a period of time."
You can find more recommendations from the CDC about Canida Auris by clicking here.

